Today I’m sharing insights into my own gut microbiome, you’re about to get to know me on a whole new level! 😂

Why? Because it’s a striking example of the effects of emotional stress on the gut.
Here’s the background. After two years of significant emotional stress, I realised that my gut had become a burial site for unresolved trauma. That’s where I held all my tension, and I really suffered for it. ⚰️
Consequently, I’d developed some uncomfortable symptoms – loose stools, bloating (looking like I was pregnant), visceral pain, severe brain fog, poor short-term memory and forgetfulness (this really troubled me).
It finally drove me to take action – so I ordered a stool test.
💩 The test: Complete Microbiome Mapping
The stool test I ran uses a single stool sample to assess the patient’s microbiome. This comprehensive report screens for pathogenic bacteria, normal gut bacteria, opportunistic pathogens, fungi, viruses and parasites.
It also measures various immune and digestive markers, such as those linked to inflammation, pancreatic function, and gluten sensitivity.
Now let’s take a look at some of the key findings…
🦠 Low immune defence
The first thing I noticed when results came back was an incredibly low level of secretory IgA (SIgA). What’s SIgA, you ask? It’s an immunoglobulin found in your mucosal surfaces—not just in the gut, but also in the sinuses, mouth, throat, lungs, bladder, and vagina.
SIgA is the primary antibody in your protective mucosal secretions, acting as an immune barrier. It binds to invading microorganisms and traps them within the gut’s mucosal layer, neutralizing them.
SIgA also tags food as acceptable, so when its levels are low, it can increase sensitivity to foods.
What suppresses SIgA production? You guessed it—stress (prolonged exposure to cortisol).
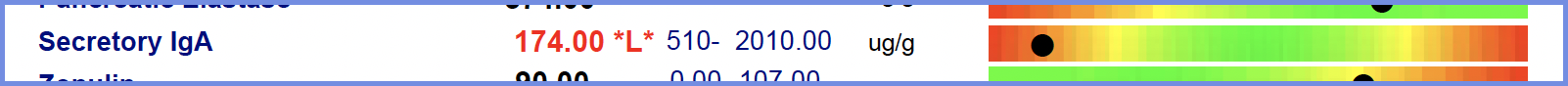
I had lost my first line of defence against pathogens, leaving me vulnerable to inflammation. And where there’s inflammation, increased intestinal permeability (leaky gut) follows.
🧫 Low beneficial microbes
The next thing that caught my eye was this:
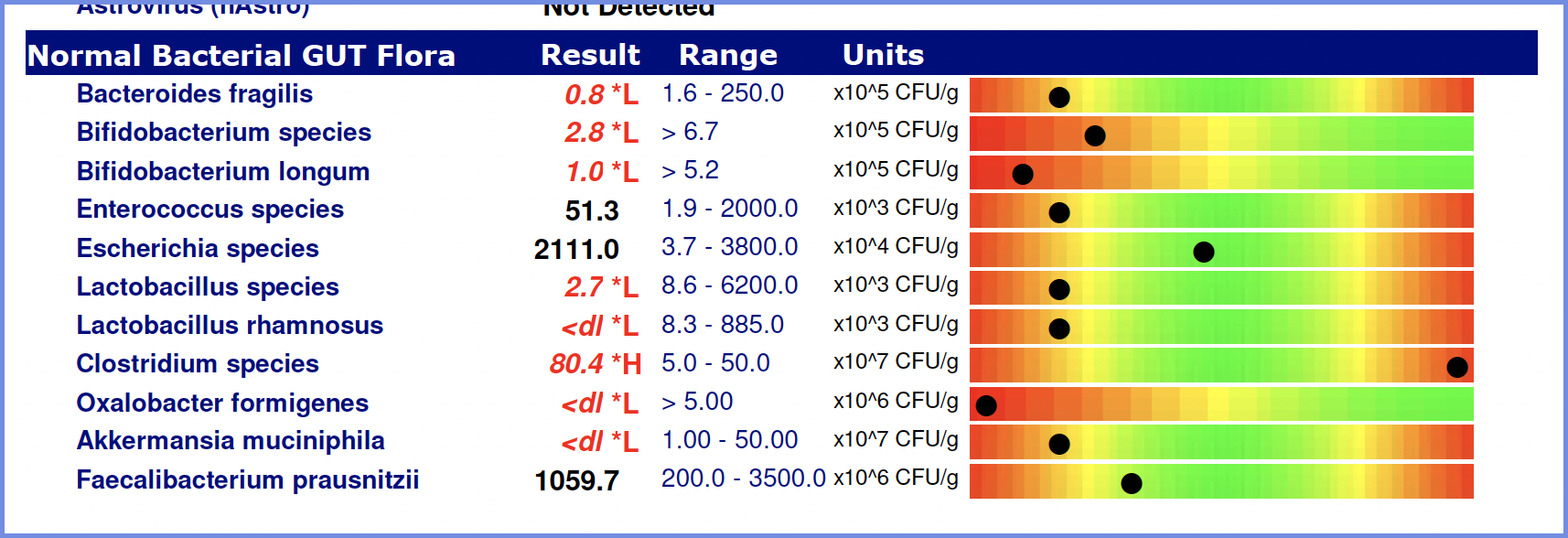
Yikes! That’s a striking deficiency of beneficial gut microbes. This isn’t due to medications, or antibiotics – this is emotional stress! This deficiency means I have low microbial diversity.
And the lower the diversity of the gut microbiome, the poorer your overall health and resilience against chronic disease.
In a healthy gut, with good diversity, bacteria produce short-chain fatty acids (SCFAs) as a by-product of metabolism. These SCFAs happen to be incredibly nourishing to the cells of the colon. Butyrate, the most researched SCFA, plays a significant role in reducing inflammation throughout the body, from the gut to the brain.
Further, this lack of diversity has implications for mental health, due to interactions between the gut-brain axis. Just one example – Lactobacillus rhamnosus modulates GABA levels in different regions of the brain, reducing excitation and improving stress, anxiety and cognition.
These results indicate that the bowel is inflamed.
🥐 Elevated immune response to gluten
Ok last standout – extremely elevated levels of a-transglutaminase IgA. These are antibodies that show an immune response to gluten.
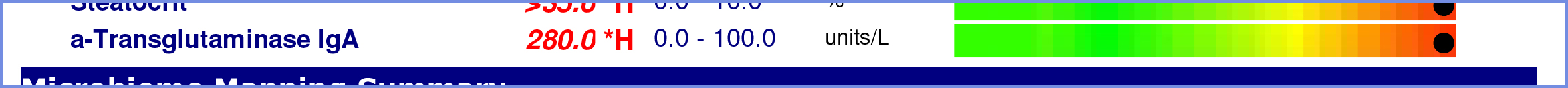
Now, I’m not actually Celiac, but this told me my immune system was reacting to gluten as if I was. This is likely due to compromised SIgA levels.
It’s a sad day when you say goodbye to sourdough.
📋Summary
All in all, my results clearly showed that prolonged exposure to stress had promoted inflammation (cue loose stools, bloating) and caused a breakdown in the integrity of the gut wall.
Stress = inflammation = breakdown of tissues.
I didn’t do an intestinal permeability test, but it’s highly likely there was some degree of leaky gut.
In leaky gut (stress is the number one cause, by the way), food antigens, such as the gliadin protein in gluten, are able to pass through the gut wall and cause widespread symptoms, like severe brain fog.
🧘♀️ How I fixed it
The reason I wanted to share this as a case study is that it really demonstrates how damaging stress is to the gut.
As long as the stress continues and blood flow and energy are diverted away from the gut, healing will remain a challenge.
You need to address the cause – reduce the stress, balance your cortisol pattern, and you’ll activate your own innate healing system 😄
Once you’ve done that, all the other wonderful interventions you bring in to support the gut will work sooo much better.
In my case, I worked hard to support my adrenals and nervous system – particularly the vagus nerve (of which has major anti-inflammatory effects within the body).
Then I worked on increasing microbial diversity via diet and prebiotics, reducing inflammation and healing the gut lining.
I hope the inner workings of my gut help give you a better sense of what might be going on in your own body – if you need support, you can book a consult here. And remember, if you really want to heal the gut, you’ve got to reduce cortisol first.
Hope that helps,
Till next time,
Lauren.





Comments +