Perimenopause is a natural transitional phase in a woman’s life, often starting up to a decade before menopause. During this time, the ovaries gradually produce less oestrogen and progesterone—think of them heading into retirement with a well-deserved mocktail in the sun!

You may experience irregular periods, dramatic hormonal swings, and a mix of physical and emotional symptoms. In many ways, it’s like puberty in reverse.
Today, I want to focus on something often overlooked: the thyroid.
The thyroid is highly sensitive to hormonal shifts during perimenopause.
These fluctuations make this a vulnerable time for triggering new autoimmune thyroid conditions—particularly in women with a genetic predisposition or a history of chronic stress—as well as worsening existing thyroid issues (hello, unexpected flare!) or tipping someone toward hypo- or hyperthyroid patterns.
Because many symptoms—fatigue, mood swings, brain fog, joint pain and weight changes—overlap between the two, they’re often written off as “just your age,” leading to missed diagnoses.
This is why perimenopause can feel extra challenging—and why it’s important not to automatically blame all your symptoms on reproductive hormones alone [Source].
The thyroid-perimenopause connection
Hormonal changes can trigger thyroid dysfunction at any age, but it often appears in midlife. Graves’ disease typically begins between ages 40–60, while Hashimoto’s is more common in late perimenopause than in younger women.
Progesterone
Progesterone is usually the first hormone to decline during perimenopause, leaving a relative excess of oestrogen.
Progesterone supports thyroid function by lowering thyroid-binding globulin (TBG), which helps more free thyroid hormone reach your cells.
As progesterone drops, this effect diminishes, potentially contributing to low thyroid symptoms in susceptible women.
With lower progesterone, we lose its calming, protective effect. This can reduce stress resilience, and over time, elevated cortisol can suppress thyroid function.
Here’s the tricky part: thyroid and ovarian hormones work hand in hand. Your ovaries need adequate thyroid hormone to produce progesterone and maintain regular cycles.
That’s why perimenopause can bring a spike in symptoms from both systems at once.
Oestrogen
Oestradiol fluctuates wildly in perimenopause, with periods of both high and low levels. These swings affect your thyroid too.
Oestrogen mainly influences thyroid function by increasing TBG, the protein that carries thyroid hormones in your blood.
When TBG is high, more hormone is “tied up” and less is free to work in your cells, which can leave you feeling tired or noticing your weight creeping up.
If you’re taking oral oestrogen (HRT), this can push TBG even higher, meaning women on thyroxine might need a slightly higher dose.
Check your thyroid function after starting oral oestrogen. Skin gels or patches don’t have this effect, so your dose usually stays the same [Source].
Another part of the story is how thyroid hormones get activated. Your body mainly produces T4, which doesn’t do much on its own until it’s turned into T3–the active form that directly influences metabolism, energy levels, and brain function.
High oestrogen levels can down-regulate the enzyme that facilitates this conversion, leading to low T3 levels – something I see often in my clients.
Autoimmune risk
Perimenopause brings changes to immune regulation as progesterone declines first, followed by increasingly erratic oestrogen signalling.
The loss of progesterone’s immune-calming effects, combined with hormonal volatility, can tip the body toward a more inflammatory, immune-reactive state. In genetically susceptible women, this may increase the risk of autoimmune thyroid conditions such as Hashimoto’s.
Symptom overlap
Fatigue
- With hypothyroidism, low thyroid hormones slow down energy production at a cellular level, so everything just feels harder
- With hyperthyroidism, your metabolism is stuck in overdrive. Many women describe it as “running a marathon while standing still,” often with broken sleep that leaves you exhausted
- In perimenopause, fatigue is often tied to poor sleep, commonly driven by falling progesterone. Progesterone has a calming effect on the nervous system and supports GABA, our feel-good, calming neurotransmitter
- Sleep disruption can increase stress hormones, which typically worsen inflammation
Weight gain
- In hypothyroidism, weight gain is due to a slower metabolism. Sluggish digestion can also mean bloating and constipation, adding to the discomfort around the waistband
- In the later stage of perimenopause, weigh gain it is typically related to insulin resistance, due to declining oestrogen
- You can be eating the same foods and exercising the same amount, and still be gaining weight (unfair, I know!)
- In both cases, this weight gain is NOT about willpower, laziness or poor food choices
Mood changes
- In hypothyroidism, it’s common to experience flat, depressed moods and lack of motivation
- In hyperthyroidism, it’s common to experience anxiety, irritability and nervousness
- In perimenopause, declining progesterone can contribute to anxiety and irritability, while fluctuating oestrogen levels are associated with an increased risk of depression
✎ᝰ.📓🗒 A 2024 meta-analysis found that women are significantly more likely (around 1.4×) to experience depression during perimenopause. Researchers describe this stage as a “window of vulnerability,” where rapid and unpredictable fluctuations in oestrogen can disrupt brain systems involved in mood regulation, stress response, and emotional resilience [Source]. ✎ᝰ.📓🗒
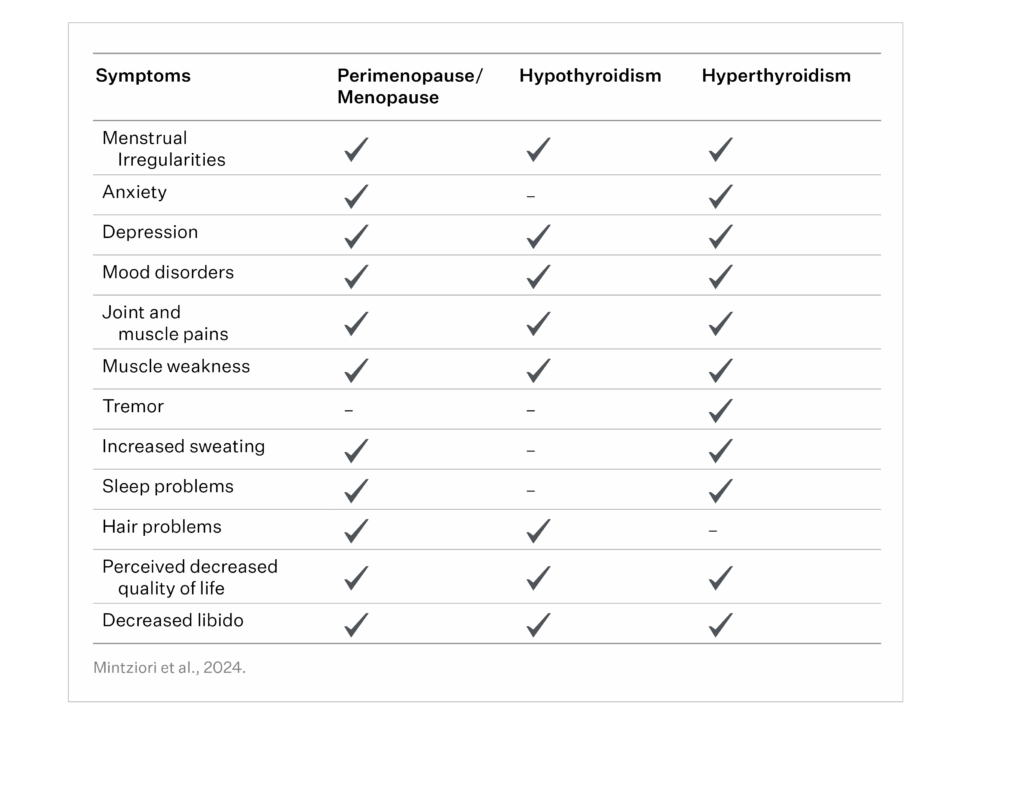
As you can see, there’s a big overlap between perimenopause and thyroid symptoms.
Fatigue, weight gain, anxiety, hair loss, low libido and more… these could be your thyroid, perimenopause, or both!
What to do
The best step is to assess your thyroid function properly. This ensures you don’t miss an underlying thyroid condition. With the right testing and guidance, many uncomfortable symptoms can be alleviated, helping you feel more like yourself again.
🥗 Lifestyle and dietary adjustments can have a powerful impact on easing symptoms from both perimenopause and thyroid issues.
Get support
If you’re struggling with fatigue, brain fog, weight changes, or mood swings during perimenopause, don’t automatically blame your ovaries. Check your thyroid. Understanding how these two systems interact can make this transitional time far less confusing—and far more manageable.
If you need holistic thyroid care, feel free to check out my Thyroid Revival package here, or book a clarity call with me to see how I can help.
Lauren. 🥑

Feeling burnt out or off your game?
It might be low iron, B12, magnesium, zinc, or vitamin D. Watch Nutrient Foundations for Energy, Mood & Resilience to learn where to start.
X




Comments +